DON’T LET SOMEONE
REMOVE YOUR MENISCUS
(OR POORLY REPAIR IT)
Save your meniscus and prevent future arthritis with the inventor of the most advanced Meniscus Repair Technique
Treatment Options: Pros & Cons
There are 1 million meniscus surgeries performed in the US per year and over 90% of them are REMOVAL surgeries called ‘partial meniscectomy’ , ‘trimming’ , ‘cleaning up’ or ‘debriding’.
Read this site to learn why is the case, and to learn your smartest option: Circumferential Repair.
Repair(sew tear together)
REPAIR
(sew tear together)
PROS
- Heals the meniscus by sewing the torn edges together
- Resolves pain generated from the meniscus tear
- Maintains the health of the knee by restoring its natural functionality
- Scientifically proven to work
CONS
- Requires minimally invasive arthroscopic surgery
- Requires 6 weeks of healing followed by a few months of physical therapy
- Cutting sports must be avoided for 5-9 months
References
Even before the advent of modern Circumferential Stitch repair techniques, the medical literature supported good results with meniscus repair
Reference 1, Reference 2, Reference 3, Reference 4, Reference 5, Reference 6, Reference 7, Reference 8,Reference 9, Reference 10, Reference 11, Reference 12
Circumferential Stitches provide enhanced biomechanical repair
Reference 1, Reference 2, Reference 3, Reference 4, Reference 5, Reference 6
Remove(“trim” or “clean up”)
REMOVE
(“trim” or “clean up”)
PROS
- Relatively quicker recovery after surgery
CONS
- Significantly reduced effectiveness of your meniscus
- Has not been shown to improve symptoms better than non-operative care when measured at 6 months and 2 years post-operatively
- Contact pressures and areas of the surrounding cartilage become increasingly compromised
- Increased risk for knee arthritis
- Increased likelihood of needing knee replacement surgery in the future
References
The knee is at increased risk for arthritis and the eventual need for total knee replacement
Reference 1, Reference 2, Reference 3, Reference 4, Reference 5, Reference 6, Reference 7, Reference 8, Reference 9
Has not been shown to improve symptoms better than non-operative care when measured at 6 months and 2 years post-operatively
Do nothing
DO NOTHING
PROS
- There is no treatment and no economic related cost
CONS
- Pain and dysfunction are very likely to persist
- Compromised contact pressures and areas of the surrounding cartilage
- Increased risk for knee arthritis
- Increased risk of needing eventual knee replacement surgery
References
Reference 1, Reference 2, Reference 3, Reference 4, Reference 5, Reference 6
Physical Therapy
PHYSICAL THERAPY
PROS
- Non-invasive
CONS
- Will not heal the tear but might help propagate the tear into a less painful state
- Compromised contact pressures and areas of the surrounding cartilage
- Increased risk for knee arthritis
Increased risk of needing eventual knee replacement surgery
Injections
INJECTIONS
PROS
- Your knee can feel better for 3-6 months at a time
CONS
- All types of injections give temporary relief via similar anti-inflammatory mechanisms
- Have not been shown to heal meniscus tears but might help propagate the tear into a less painful state
- Compromised contact pressures and areas of the surrounding cartilage
- Increased risk for knee arthritis
- Increased risk of needing eventual knee replacement surgery
(sew tear together)

(“trim” or “clean up”)

(sew tear together)

(sew tear together)

(sew tear together)

REPAIR
(sew tear together)
PROS
- Heals the meniscus by sewing the torn edges together
- Resolves pain generated from the meniscus tear
- Maintains the health of the knee by restoring its natural functionality
- Scientifically proven to work
CONS
- Requires minimally invasive arthroscopic surgery
- Requires 6 weeks of healing followed by a few months of physical therapy
- Cutting sports must be avoided for 5-9 months
References
Even before the advent of modern Circumferential Stitch repair techniques, the medical literature supported good results with meniscus repairREMOVE
(“trim” or “clean up”)
PROS
- Relatively quicker recovery after surgery
CONS
- Significantly reduced effectiveness of your meniscus
- Has not been shown to improve symptoms better than non-operative care when measured at 6 months and 2 years post-operatively
- Contact pressures and areas of the surrounding cartilage become increasingly compromised
- Increased risk for knee arthritis
- Increased likelihood of needing knee replacement surgery in the future
References
The knee is at increased risk for arthritis and the eventual need for total knee replacementDO NOTHING
PROS
- There is no treatment and no economic related cost
CONS
- Pain and dysfunction are very likely to persist
- Compromised contact pressures and areas of the surrounding cartilage
- Increased risk for knee arthritis
- Increased risk of needing eventual knee replacement surgery
References
PHYSICAL THERAPY
PROS
-
- Non-invasive
CONS
- Will not heal the tear but might help propagate the tear into a less painful state
- Compromised contact pressures and areas of the surrounding cartilage
- Increased risk for knee arthritis
- Increased risk of needing eventual knee replacement surgery
INJECTIONS
PROS
-
- Your knee can feel better for 3-6 months at a time
CONS
- All types of injections give temporary relief via similar anti-inflammatory mechanisms
- Have not been shown to heal meniscus tears but might help propagate the tear into a less painful state
- Compromised contact pressures and areas of the surrounding cartilage
- Increased risk of needing eventual knee replacement surgery
- Increased risk for knee arthritis
- Increased risk of needing eventual knee replacement surgery

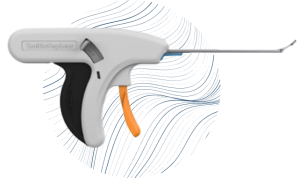
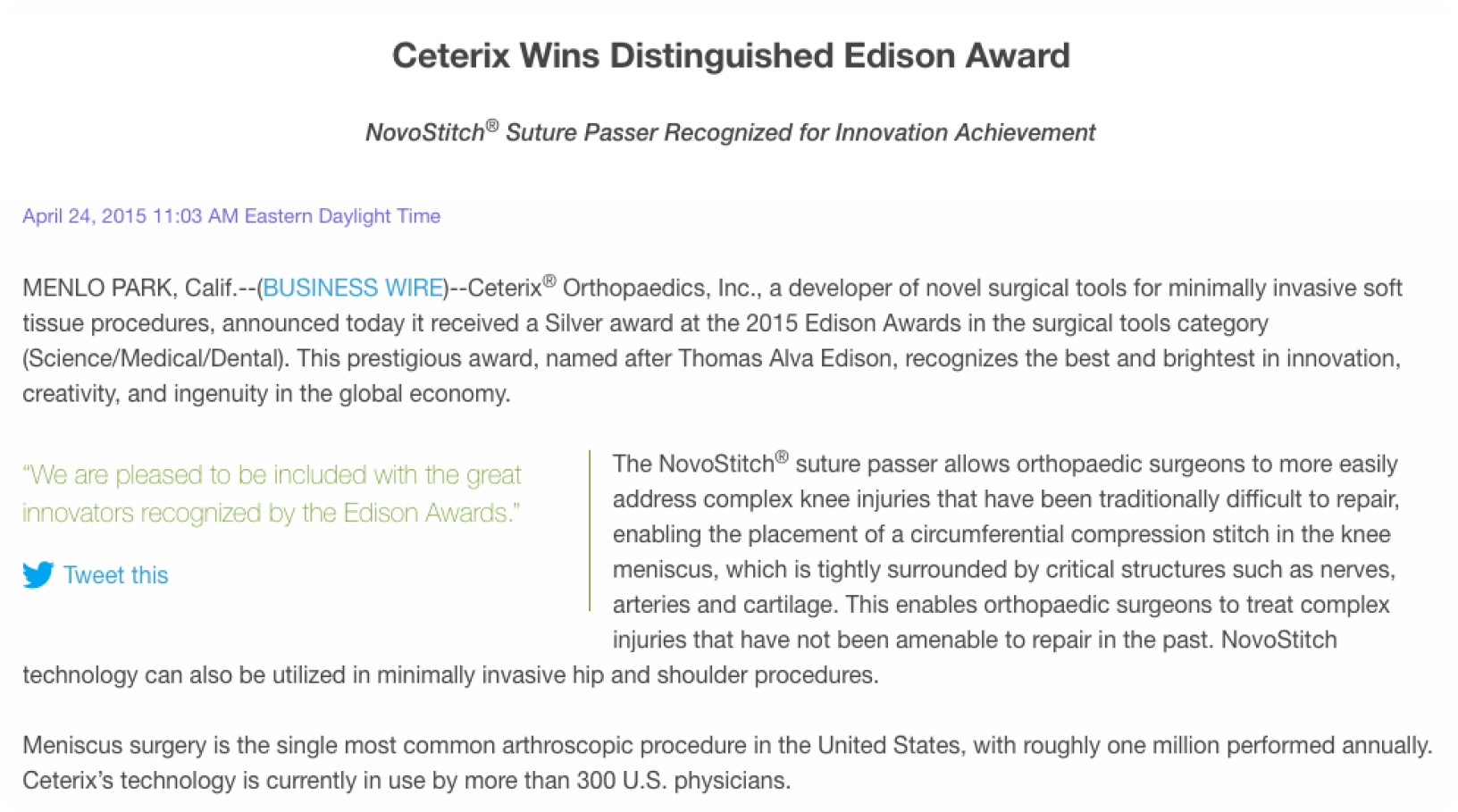
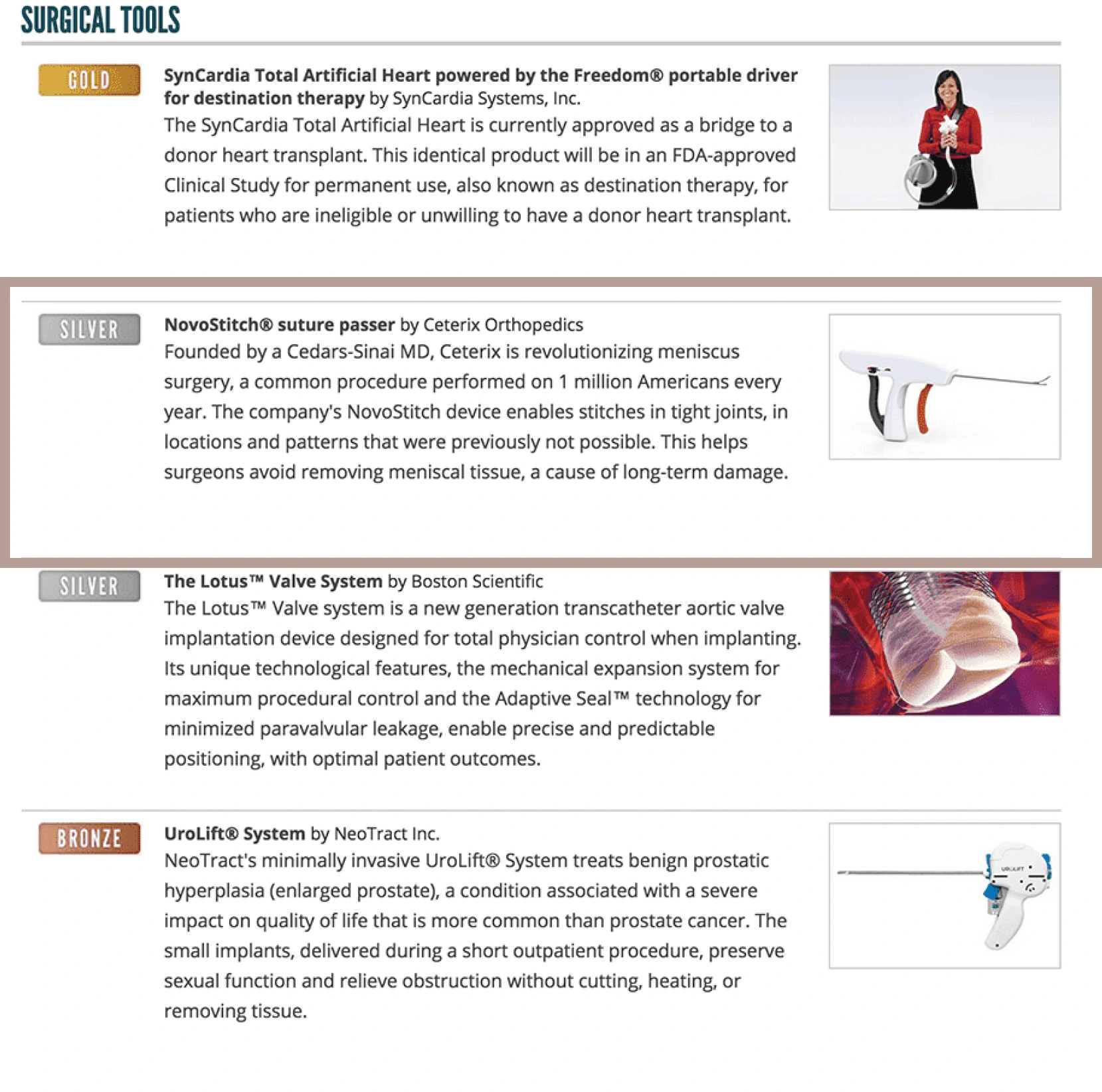
Meet the award-winning surgeon and inventor of the most modern Meniscal Repair System:
Dr. Justin Saliman, is a Stanford trained orthopedic surgeon who invented the Edison Award winning “Novo Stitch Pro Meniscal Repair System” and the “Circumferential Stitching” technique.
This unique treatment allows him to arthroscopically sew all meniscus tear types including those previously considered difficult or impossible to sew back together.
As a result, patients heal pain and dysfunction while preventing arthritis in the long-term.
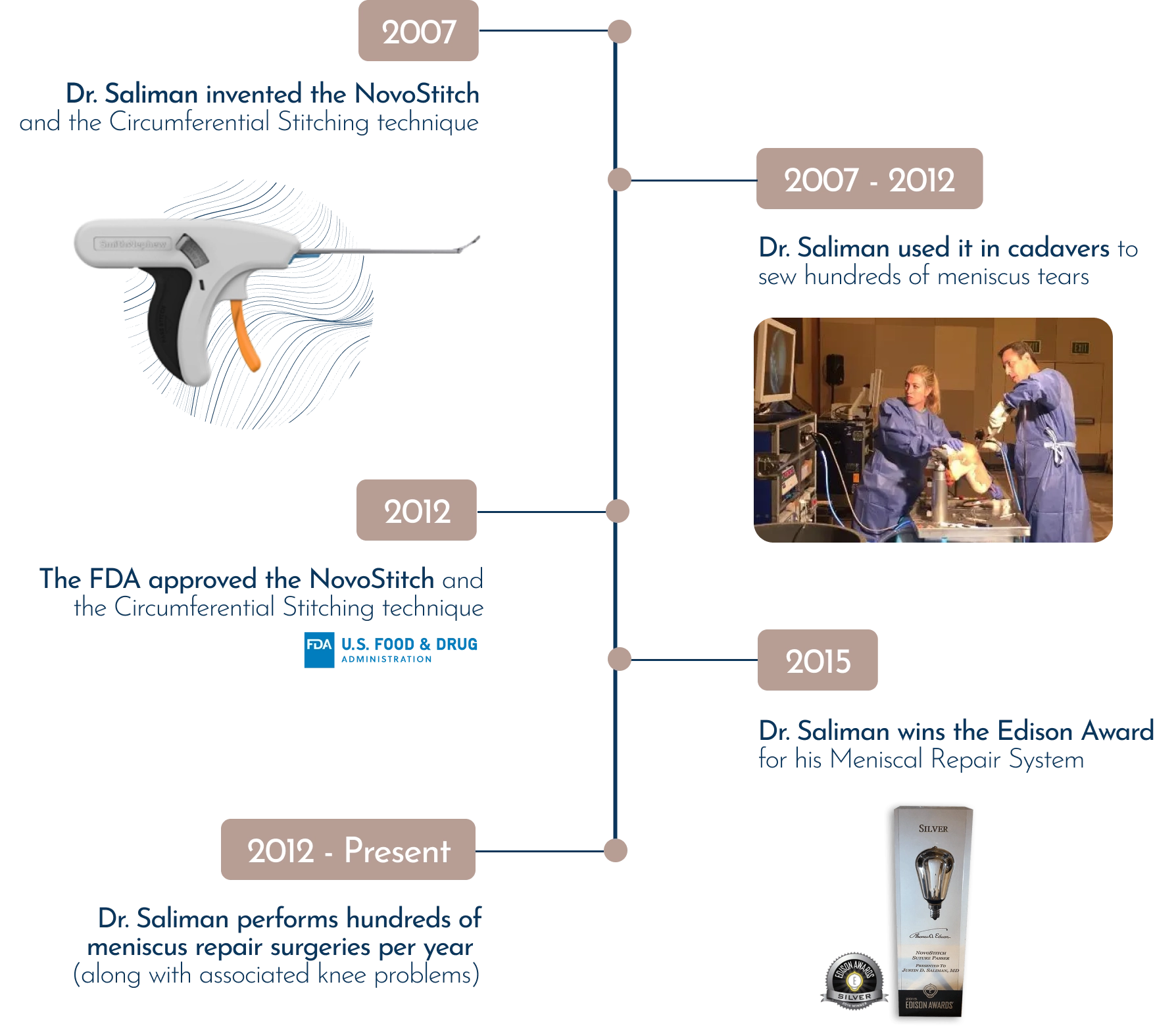
2012 - Present
Dr. Saliman performs hundreds of meniscal repair surgeries a year with 90% success rate
Holding over 25 patents on meniscus repair, no one has more experience sewing meniscus tears back together!
Why Circumferential Stitching Repair
is the best treatment for meniscus tears
It takes 6 weeks for musculoskeletal tissues to heal. During this time, the meniscus
tear edges must be firmly held together as there are too many knee forces acting on the tear and constantly pulling it apart. Tears do not heal on their own nor with any type of injection or therapy.
They must be securely sewn.
Circumferential Technique
is biomechanically stronger
Dr. Saliman’s NovoStitch medical device allows surgeons to place circumferential sutures around meniscus tears – providing uniform, anatomic compression of the tear edges.
Old Techniques
are riskier and incomplete
Traditional techniques only effectively sew together the top part of the tear, leading to partial healing and increased risk of meniscus re-tears.
Almost all meniscus tear types are repairable and
best treated with the Circumferential Repair System
Dr. Saliman’s advanced meniscal repair system can sew together even horizontal, radial, oblique, and other complex tears that were previously thought “imposible” to repair.
The Medical Literature Supports Repair, Not Removal
Even before modern Circumferential Stitch repair techniques, the medical literature supported good results with meniscus repair
Circumferential Stitches provide enhanced
biomechanical repair:
Consequences of doing nothing
Consequences of removing or trimming meniscus
Removing or trimming meniscus has not been shown to improve symptoms better than non-operative care
Dr. Saliman tracks all of his patients’ outcomes for 5 years
Dr. Saliman measures all of his patients’ symptoms and knee-related quality of life before and after surgery.
This allows him to track how they change over time.
Outcome Tracking Certified
While all doctors should be doing this, the vast majority do not objectively measure and keep track of this data, so they don’t really know what about their treatments does and does not work.
Below are some examples of Dr. Saliman’s great results. Each tile displays a patient’s initial and latest follow-up scores, which are independently measured and authenticated by a software called OutcomeMD.
Why do most surgeons
prefer to trim or remove the meniscus?
and why you should save it
Lack of economic incentives and poor training account for why
most surgeons unfortunately decide to trim, remove or partially mitigate symptoms.

Circumferential repair is difficult
Circumferential stitch repair is quite hard to do and requires specialized training. Using the NovoStitch is like rubbing your belly and patting your head, and each stitch requires arthroscopic knot tying, a skill most knee surgeons infrequently perform. Stitches should be placed every 5mm or so, which means to do a good job the surgeon will need to place several stitches and tie several knots. And managing the sutures to get optimal placement in all zones can be very confusing for surgeons who don’t have years of experience with this technique.

Meniscus repair does not pay well
Meniscus repair is one of the poorest paying procedures an orthopaedic surgeon can do. As a result surgeons don’t put in the long hours (or years) of practice necessary to become facile at placing circumferential compression stitches for complex meniscus tears. Furthermore, some of the surgery centers will not allow the surgeon to put in enough stitches because the cost of each stitch can in some cases mean the surgery center will lose money on the case.

Once bitten twice shy
Older repair techniques are much easier to perform but are less effective at anatomically reducing and uniformly compressing the torn edges during healing. This is especially true of tears that involve the tibial (bottom) side of the meniscus or that are not classic vertical peripheral third tear patterns. Surgeons who use old techniques struggle to place adequate stitches in the middle third (‘red-white’) zone and on the bottom side of the tears, hence they have seen failure of their repairs, leading them to believe the meniscus can’t heal when in reality the failures are typically from inadequate sewing.

It’s easier to sell meniscus removal
Patients don’t need rehab and can more quickly return to sports when you remove their meniscus. There’s also no need for bracing. Surgeons explain meniscus removal surgery as ‘quick and easy’, and patients love that, but at what cost?

Injections & replacement pay well
When arthritis sets in from not having a functional meniscus (from either leaving it torn or having it removed), the patient usually returns to the same doctor. That doctor profits from giving regular injections to mitigate pain (the only effect of all injection types) and from performing the eventual knee replacement surgery.

Risk of injuring nerves & arteries
Traditional repair techniques involve needle penetration beyond the capsule into the back of the knee which has been shown to risk catastrophic injury. Other times it causes significant pain in the back of the knee after surgery. Either way, it’s best to avoid risk of neurovascualr injury. The NovoStitch does not require needle penetration toward the neurovascular structures.
Most common “excuse”
“It won’t heal because...”

“Only the peripheral third has a blood supply”
Here’s a list of papers proving that the area of the meniscus that ‘doesn’t have a good blood supply’ (typically the central and middle third of the meniscus) can in fact heal. These zones are just harder to repair with traditional techniques.

“Your tear is degenerative or complex”
Prior to Dr. Saliman’s NovoStitch, there was no good way to sew horizontal, intrasubstance, radial, flap and complex meniscus tears. Because these tear types often occur slowly over time (as opposed to an acute trauma) doctors often call them ‘degenerative’. However when properly sewn together in an otherwise healthy knee, they heal great!
Your Roadmap to recovery:
Navigating the Post-Op Timeline
 Transportation
Transportation
FLYING
Most patients can fly out the same or the next day.
DRIVING
You will be able to drive if and when you are off all pain medications (except anti-inflammatories), you feel it is safe to do to so, and you feel comfortable hitting the brakes hard if needed.
 The day of sugery
The day of sugery
Dr. Saliman operates out of a Cedars-Sinai owned surgery center in Beverly Hills called Precision ASC.
Dr. Saliman does a plastic surgery closure for the small incisions and there are no stitches to take out. One day after surgery you can remove the brace and ACE bandage and take a shower. There will be a waterproof dressing underneath the ACE bandage that should remain in place until 7 days after surgery, at which time you can remove it and continue to shower normally.
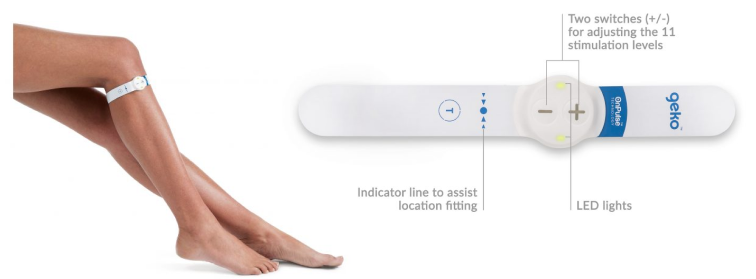
Blood clots are very uncommon after meniscus repair sugery, however to further reduce your risk,, you will have a small sticker on the outside lower part of your knee. This is a neuromuscular electrostimulation technology named Geko. It will stimulate your calf muscle for around 30 hours after surgery. If the stimulation is bothering you there is a minus button which lets you turn it down.
 First 6 weeks after surgery
First 6 weeks after surgery
HORIZONTAL, BUCKET HANDLE, VERTICAL, INTRASUBSTANCE, AND COMPLEX TEARS
Immediately after surgery you will be able to walk with a hinged knee braced locked in extension (the brace is typically covered by insurance). NO need for crutches.

For the next 6 weeks after surgery, you will be required to wear this knee braced locked in extension during weight-bearing.
During this period of time, you will be able to unlock the knee brace and allow your knee to bend to 90 degrees when not bearing weight.
Note: It is highly important that you do not place weight across a bent knee until your surgeon allows you to do so, as the repair needs enough time to heal before tolerating it.
RADIAL AND ROOT TEARS
In order for the repaired meniscus to properly heal, you will be typically required to NOT bear weight for 6 weeks after surgery.
A knee brace is not required for radial or root tear repairs.
ISOMETRIC QUAD EXERCISES
To avoid losing muscle strength, perform Isometric quad exercises as directed in your post-op instructions provided by Dr. Saliman
 Follow up visits
Follow up visits
You will have a follow up consultation a week after surgery. At this visit you will be given a physical therapy prescription, rehab protocol and a copy of the operative report. You will also have a follow up visit after you have completed about 6 weeks of physical therapy to make sure you are on course. Dr. Saliman will be reachable throughout your healing journey. If you live far away or out-of-state your visits can be via telephone or Dr. Saliman’s HIPAA compliant zoom.
 Physical Therapy
Physical Therapy
Due to the brace and/or non-weight bearing status, your quadriceps and hamstrings will become very weak. So no matter the type of tear, 6 weeks after surgery you will need to start physical therapy to regain your motion and strengthen your leg.
Dr. Saliman will give you a particular protocol for you and your physical therapist to follow after surgery.
 Returning to cutting sports
Returning to cutting sports
This is usually allowed 4-9 months after surgery.
 Outcome Tracking
Outcome Tracking
Dr. Saliman measures and follows all of his patients’ outcomes for several years after surgery using a unique software to objectively report your progress called OutcomeMD.
Patients fly in from all over the world.
Would you like to connect with one?
Have Dr. Saliman connect you with a patient who had their meniscus repaired.
Experience the relief of the Circumferential
Meniscus Repair System
Frequently Asked Questions
But I was told the meniscus doesn’t have a good blood supply?
The area of the meniscus that ‘doesn’t have a good blood supply, typically the central and middle third of the meniscus, can, in fact, heal. These zones are just harder to repair with traditional techniques. And the central third can be removed as it has not been shown to be critical to the knee’s long-term health. So what’s really important is to have any tears that occur in the middle or peripheral third repaired (assuming the knee is not already arthritic, in which case the options are conservative treatment or knee replacement surgery). Below are papers demonstrating that the avascular zone can, in fact, heal, and these papers were published even before the Circumferential Stitch for meniscus repair enabled improved mechanical repairs.
References:
1. Avascular Zone Meniscal Repair in ACL patients, 79% completely healed.Ahn, J.H., et al., Clinical and second-look arthroscopic evaluation of repaired medial meniscus in anterior cruciate ligament-reconstructed knees. Am J Sports Med, 2010. 38(3): p. 472-7.
2. Avascular Zone Isolated Meniscal Tears, horizontal sutures, 60% completely healed.Eggli, S., et al., Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. Am J Sports Med, 1995. 23(6): p. 715-20.
3. Avascular Zone, including radial tears, patients over 40 yrs, 87% success rate.Noyes, F.R. and S.D. Barber-Westin, Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 2000. 16(8): p. 822-829.
4. Avascular Zone, vertical sutures, under 20yrs, 62% success rate.Noyes, F.R., et al., Greater Than 10-Year Results of Red-White Longitudinal Meniscus Repairs in Patients 20 Years of Age or Younger. The American Journal of Sports Medicine, 2011.
5. Avascular Zone, vertical sutures in ACL patients, 54% success rate.Asahina, S., et al., Intermediate-Term Results of Meniscal Repair in Anterior Cruciate Ligament-Reconstructed Knees. The American Journal of Sports Medicine, 1998. 26(5): p. 688-691.
6. Avascular Zone, vertical sutures, 94% success rate.Barber, F.A., D.H. Johnson, and J.L. Halbrecht, Arthroscopic Meniscal Repair Using the BioStinger. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 2005. 21(6): p. 744-750.
7. Avascular Zone, vertical sutures, 100% success, arrow fixator, 80%.Steenbrugge, F., et al., Arthroscopic meniscus repair: inside-out technique vs. Biofix meniscus arrow. Knee Surgery, Sports Traumatology, Arthroscopy, 2004. 12(1): p. 43-49.
8. Avascular Zone, vertical sutures, 79% success.Buseck, M.S. and F.R. Noyes, Arthroscopic evaluation of meniscal repairs after anterior cruciate ligament reconstruction and immediate motion. The American Journal of Sports Medicine, 1991. 19(5): p. 489-494.
9. Avascular Zone, vertical sutures, radial tears 73% success, flap tears 78% success. Rubman, M.H., F.R. Noyes, and S.D. Barber-Westin, Arthroscopic Repair of Meniscal Tears that Extend into the Avascular Zone. The American Journal of Sports Medicine, 1998. 26(1): p. 87-95.
10. Avascular Zone, All inside circumferential suture, 100% success.Yoo, J.C., et al., Suturing complete radial tears of the lateral meniscus. Arthroscopy, 2007. 23(11): p. 1249 e1-7.
11. Avascular Zone, all inside devices, isolated meniscal tears, 68% success.Gallacher, P.D., et al., White on white meniscal tears to fix or not to fix? The Knee, 2010. 17(4): p. 270-273.
12. Avascular Zone, vertical sutures, bucket handle tears with ACL. 91% success. Feng, H., et al., Second-Look Arthroscopic Evaluation of Bucket-Handle Meniscus Tear Repairs With Anterior Cruciate Ligament Reconstruction: 67 Consecutive Cases. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association, 2008. 24(12): p. 1358-1366.
I was told I was too old for meniscus repair?
The below studies suggest patient age may not be a significant factor.
1. Noyes, FR, Barber-Westin SD. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16(8):822-9. View study
2. Rothermel, et al. Are Outcomes After Meniscal Repair Age-Dependent? A Systematic Review. Arthroscopy. 2017 Dec. 19 epub. ahead of print. View study
3. Steadman, et al. Meniscus suture repair: minimum 10-year outcomes in patients younger than 40 years compared with patients 40 and older. AJSM. 2015 Sep;43(9):2222-7. View study
Why not just my knee replaced?
Knee replacements work well when there are no other options but have potentially devastating complications (infection, DVT, pneumonia, and blood loss leading to heart attack). Also, they don’t last forever. Every 20 years or so, patients must undergo revision surgery and lose bone mass each time. Second and third revision surgeries have dramatically increased risks of complications. Prevention via meniscus repair should be the gold standard of treatment if your knee is not already arthritic.
But I live out of state?
Patients fly in for surgery frequently. If you are out of state please book a Zoom consult.
What is a Meniscus?
Your menisci are two wedge-shaped pieces of cartilage that function to evenly distribute forces in your knee joints and effectively act as shock absorbers every time you take a step. Your menisci are critical to the long-term health of your knee, and any simple wrong position or twist can lead to a meniscus tear. When the function of your meniscus is compromised, your knee is at a high risk of becoming progressively painful and arthritic. The only definitive treatment for an arthritic knee is total knee replacement – so, SAVE YOUR MENISCUS!
Do I need cold therapy?
What is a Meniscus Tear?
A meniscus tear is a common knee injury frequently caused by everyday activities that put pressure on the knee joint, such as squatting to pick something up or getting in and out of a car. Meniscus tears may cause pain, clicking and/or the sensation of your knee getting stuck or giving out. In some cases they can also cause swelling and/or limited motion. You may still be able to walk after you tear your meniscus, and in fact, many athletes continue to play with a meniscal tear, albeit with pain and decreased function.
Does Dr. Saliman have outcome data on how patients do in his hands?
Yes, Dr. Saliman follows all of his outcomes using literature validated, objective Patient-Reported Outcome assessments via a software called OutcomeMD. He measures and tracks all outcomes and decides when and on whom to perform surgery based on the long-term outcomes of all other patients who have had similar surgeries in his hands.
Where does Dr. Saliman do surgery?
At a Cedars-Sinai-owned surgery center in Beverly Hills that is in-network with most PPO insurance plans.
What insurance does Dr. Saliman take?
- Aetna PPO
- Anthem PPO
- Blue Cross PPO
- Blue Shield PPO
- Cigna PPO
- United Healthcare PPO
- HealthNet PPO
Does Dr. Saliman still do hip and shoulder arthroscopic surgery?
He does still do arthroscopic surgery within the shoulder and hip joints.
Contact Us
Send a message to Justin D. Saliman, MD
If you have any questions, concerns, or comments regarding Dr. Justin Saliman or your knee
condition, please fill out the short contact form below
 +1(310)7035819
+1(310)7035819